New research conducted by clinical investigators at Indiana University School of Medicine in collaboration with colleagues in Uganda has shown that hydroxyurea can effectively reduce infections in children with sickle cell anemia. This breakthrough provides substantial evidence of the treatment’s efficacy and has the potential to reduce mortality rates among children in Africa, where the burden of this disease is highest.
Recently published in the journal Blood, the research reveals that treatment with hydroxyurea resulted in a remarkable 60% reduction in severe or invasive infections, including malaria, bacteremia, respiratory tract infections, and gastroenteritis, among children in Uganda diagnosed with sickle cell anemia.
“This investigation provides compelling evidence for the use of hydroxyurea in children with sickle cell anemia in Africa,” said Dr. Chandy John, co-lead investigator of the study and the Ryan White Professor of Pediatrics at IU School of Medicine. “Given the high rates of infection in this region, we hope our findings will encourage ministries of health to continue supporting and expanding access to hydroxyurea for young patients who can greatly benefit from this treatment.”
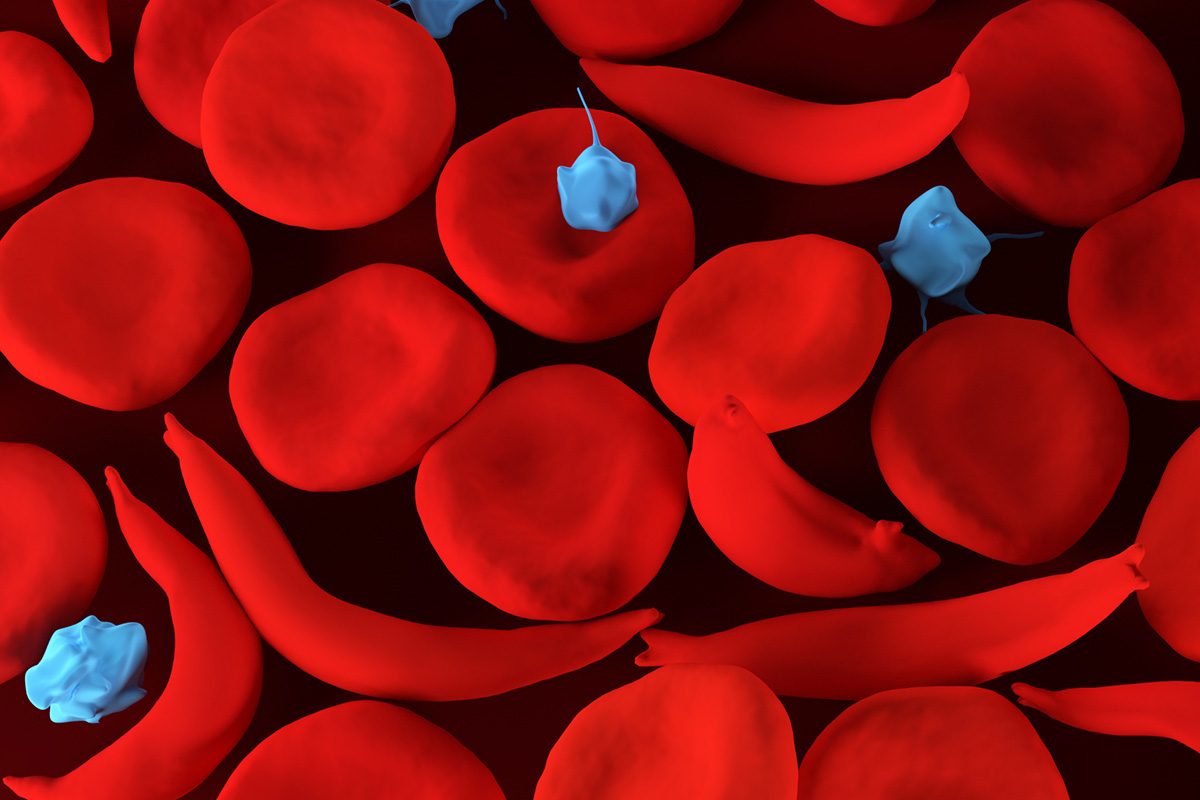
Sickle cell anemia is a genetic blood disorder that affects the structure of red blood cells, thereby impairing oxygen distribution throughout the body. This increases vulnerability to serious health complications and life-threatening infections. According to the World Health Organization, over 300,000 children worldwide are born with sickle cell disease each year, with a particularly high prevalence in African countries.
Although hydroxyurea has been approved as a treatment for sickle cell disease in children by the U.S. Food and Drug Administration since 2017, its availability and acceptance in Africa remain limited. Recognizing the growing recognition of hydroxyurea’s effectiveness in treating sickle cell-related complications in African countries, Dr. John and his colleagues identified a knowledge gap regarding the treatment’s impact on infections. Consequently, the research team incorporated hydroxyurea treatment and analysis into their existing clinical trial, Zinc for Infection Prevention in Sickle Cell Anemia.
During the study, the researchers investigated the effects of hydroxyurea on 117 children in Uganda, with a focus on various types of infections. The results demonstrated a significant decrease in the incidence of these infections following hydroxyurea treatment. Additionally, out of the nine deaths that occurred during the trial, eight were children whose parents declined hydroxyurea treatment. The only death that occurred in a child receiving hydroxyurea treatment happened just four days after starting the treatment, suggesting insufficient time for hydroxyurea to take effect.
Of the five children for whom the cause of death was known, all five died from infectious causes. The high mortality rate observed in the study, despite the expert clinical care provided by study personnel, emphasizes the urgent need for additional interventions to reduce mortality rates among children with sickle cell disease in Africa.
Dr. Ruth Namazzi, site principal investigator, first author of the study, and a lecturer in the Department of Pediatrics and Child Health at Makerere University in Uganda, explained that infections often precede other sickle cell-related complications and frequently result in hospitalizations that can be fatal. She believes that making hydroxyurea treatment the standard of care for sickle cell anemia across Africa will not only decrease the incidence of infections but, more importantly, save countless lives.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it