Telestroke Services involves the use of telemedicine technologies to connect stroke experts at specialized stroke centers, known as hub hospitals, with community hospitals that may have limited access to acute stroke expertise, known as spoke hospitals. Through telestroke, specialist doctors at hub hospitals can examine patients remotely at spoke hospitals using videoconferencing equipment and provide immediate recommendations for treatment and transfer if needed. This allows spoke hospitals to leverage specialist expertise for time-critical decisions even if an on-site neurologist is not available.
Benefits of Telestroke
Timely Treatment
One of the biggest benefits of Telestroke Services is that it enables timely treatment of acute stroke. Stroke is considered a medical emergency and treatment within the first few hours, known as the golden hour, can significantly impact outcomes. Telestroke allows specialists to evaluate patients and recommend treatments like thrombolysis even before the patient needs to be transferred to a specialized stroke center. This crucial time savings can translate to better clinical outcomes.
Expanded Access to Care
Telestroke helps expand access to acute stroke expertise for communities located far from specialized stroke centers. An estimated 60-80% of US hospitals do not have 24/7 neurology coverage needed for acute stroke management. Telestroke bridges this gap by enabling remote consultations from hub hospitals. This is extremely valuable for rural and underserved areas with limited local stroke resources.
Improved Stroke Recognition and Diagnosis
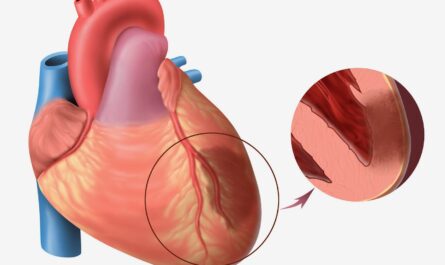
General physicians at spoke hospitals may have less experience diagnosing and differentiating between different types of strokes compared to neurologists. Through telemedicine, neurologists can use their specialized skills to accurately diagnose stroke subtypes like ischemic vs hemorrhagic strokes based on scans and patient history. This leads to more appropriate treatment choices.
Cost Savings and Resource Utilization
By facilitating timely decisions on treatments and transfers, telestroke may help reduce hospital costs associated with acute stroke care. Early administration of thrombolysis has been shown to reduce the need for intensive care, length of stay and post-stroke disability costs. Telestroke requires upfront infrastructure investment but saves on longer term costs of chronic disability care. It also optimizes ambulance and hospital bed utilization between spoke and hub facilities.
Telestroke Workflow
The typical steps involved in a telestroke consultation are:
– A patient suffering suspected acute stroke symptoms arrives at the emergency department of a spoke hospital.
– The ED physician conducts initial assessments and scans to identify if it is indeed an acute stroke.
– A telestroke cart equipped with a high-definition video camera is wheeled to the patient’s bedside.
– The hub hospital neurologist connects remotely via secure video interface to evaluate the patient, examine scans and discuss the case with the local team.
– The neurologist makes immediate treatment recommendations including administration of thrombolysis if eligible or preparing for an emergency transfer with a neuro-interventionalist or stroke unit care.
– They may also help differentiate between hemorrhagic vs ischemic strokes, assess severity and provide prognosis.
– Once the consultation ends, the local team executes treatment/transfer plan advised by the neurologist.
– The hub neurologist documents the encounter and outcomes in both hospital records.
Implementation Challenges
While telestroke offers clear clinical and access advantages, there are some challenges faced during its implementation:
– Upfront costs of requisite telemedicine equipment, network infrastructure and IT support are substantial.
– Changes to workflows and staff responsibilities require training and buy-in at both spoke and hub facilities.
– Reimbursement policies do not always cover the full range of telestroke services discouraging widespread adoption.
– Image quality during remote video evaluation is inferior to physical examination, though diagnostic accuracy is still high.
– Legal and liability aspects of telemedicine also need clear policies to be resolved.
Overcoming such implementation hurdles would require stakeholder collaborations, pilot programs, revised payment models and updated guidelines to fully realize telestroke’s promise. Overall though, it is transforming access to time-critical stroke care, especially for underserved communities.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it