Researchers from Roswell Park Comprehensive Cancer Center and Moffitt Cancer Center have developed a strategy to identify lymphoma patients at risk for poor outcomes from CAR T-cell therapy prior to treatment. The findings, published in Blood Cancer Discovery, suggest that two common and easily measured blood tests can determine the patients who are most likely to have adverse effects and not respond to CD19-targeted CAR T-cell therapy.
CAR T-cell therapy, or chimeric antigen receptor T-cell therapy, has been approved by the FDA for the treatment of various blood cancers, including lymphoma, leukemia, and multiple myeloma. While these groundbreaking therapies have shown promising results in targeting and eliminating cancer cells, they can also cause significant side effects.
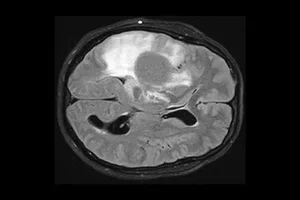
The study involved 146 patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) who had previously received multiple lines of therapy for lymphoma. After undergoing CAR T-cell therapy with axicabtagene ciloleucel (axi-cel), nearly all patients (93%) experienced cytokine release syndrome (CRS), and the majority (61%) developed immune effector cell-associated neurotoxicity syndrome (ICANS).
The research team discovered that two blood tests, c-reactive protein (CRP) and ferritin, could accurately identify patients at high risk for poor outcomes. Patients with baseline levels of CRP of at least 4 mg/dL and ferritin of 400 ng/mL or higher were found to have reduced progression-free and overall survival rates, as well as higher rates of severe toxicities.
Previously, there were no widely available lab tests or biomarkers to identify patients at high risk for poor outcomes before CAR T-cell infusion. However, the results of this study provide a method for predicting which patients are more likely to have adverse effects and not respond well to CAR T-cell therapy.
Co-senior author, Marco Davila, MD, Ph.D., Senior Vice President, and Associate Director for Translational Research at Roswell Park, expressed excitement about the findings. The research not only helps to improve CAR T-cell therapies for patients with hard-to-treat cancers but also helps identify patients who may not benefit from additional medications they do not need.
Identifying patients at high risk for poor outcomes prior to CAR T-cell therapy allows healthcare professionals to optimize treatment strategies and potentially improve the safety and efficacy of this innovative immunotherapy. With further development and validation, these blood protein tests could become a valuable tool in personalized medicine for lymphoma patients.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it